Topic 9.2. Management strategies for scoliosis in Friedreich ataxia
This chapter of the Clinical Management Guidelines for Friedreich Ataxia and the recommendations and best practice statements contained herein were endorsed by the authors and the Friedreich Ataxia Guidelines Panel in 2022.
Topic Contents
9.2. Management strategies for scoliosis in Friedreich ataxia
9.2.1 Investigation of scoliosis
9.2.2 Interventions for scoliosis
9.2.3 Conclusion
See also – 9.3 Management strategies for foot deformity in Friedreich ataxia
9.3.1 Surgery
9.3.2 Ankle foot orthotics
Disclaimer / Intended Use / Funding
Disclaimer
The Clinical Management Guidelines for Friedreich ataxia (‘Guidelines’) are protected by copyright owned by the authors who contributed to their development or said authors’ assignees.
These Guidelines are systematically developed evidence statements incorporating data from a comprehensive literature review of the most recent studies available (up to the Guidelines submission date) and reviewed according to the Grading of Recommendations, Assessment Development and Evaluations (GRADE) framework © The Grade Working Group.
Guidelines users must seek out the most recent information that might supersede the diagnostic and treatment recommendations contained within these Guidelines and consider local variations in clinical settings, funding and resources that may impact on the implementation of the recommendations set out in these Guidelines.
The authors of these Guidelines disclaim all liability for the accuracy or completeness of the Guidelines, and disclaim all warranties, express or implied to their incorrect use.
Intended Use
These Guidelines are made available as general information only and do not constitute medical advice. These Guidelines are intended to assist qualified healthcare professionals make informed treatment decisions about the care of individuals with Friedreich ataxia. They are not intended as a sole source of guidance in managing issues related to Friedreich ataxia. Rather, they are designed to assist clinicians by providing an evidence-based framework for decision-making.
These Guidelines are not intended to replace clinical judgment and other approaches to diagnosing and managing problems associated with Friedreich ataxia which may be appropriate in specific circumstances. Ultimately, healthcare professionals must make their own treatment decisions on a case-by-case basis, after consultation with their patients, using their clinical judgment, knowledge and expertise.
Guidelines users must not edit or modify the Guidelines in any way – including removing any branding, acknowledgement, authorship or copyright notice.
Funding
The authors of this document gratefully acknowledge the support of the Friedreich Ataxia Research Alliance (FARA). The views and opinions expressed in the Guidelines are solely those of the authors and do not necessarily reflect the official policy or position of FARA.
9.2. Management strategies for scoliosis in Friedreich ataxia
John Flynn, David Lynch and Louise Corben
9.2.1 Investigation of scoliosis
The usual method of investigation of scoliosis is antero-posterior and lateral full spine radiographs either standing or supine. However, Allard and colleagues (9) suggest this may lead to inconsistent measurement and recommends the use of a rotational booth. The Cobb method (18) is used to determine the degree of curve. Pelvic obliquity is defined as the angle between a line joining both iliac crests and a line intersecting the middle of the pedicles of L4 and L5 on the posteroanterior view (7, 19).
9.2.2 Interventions for scoliosis
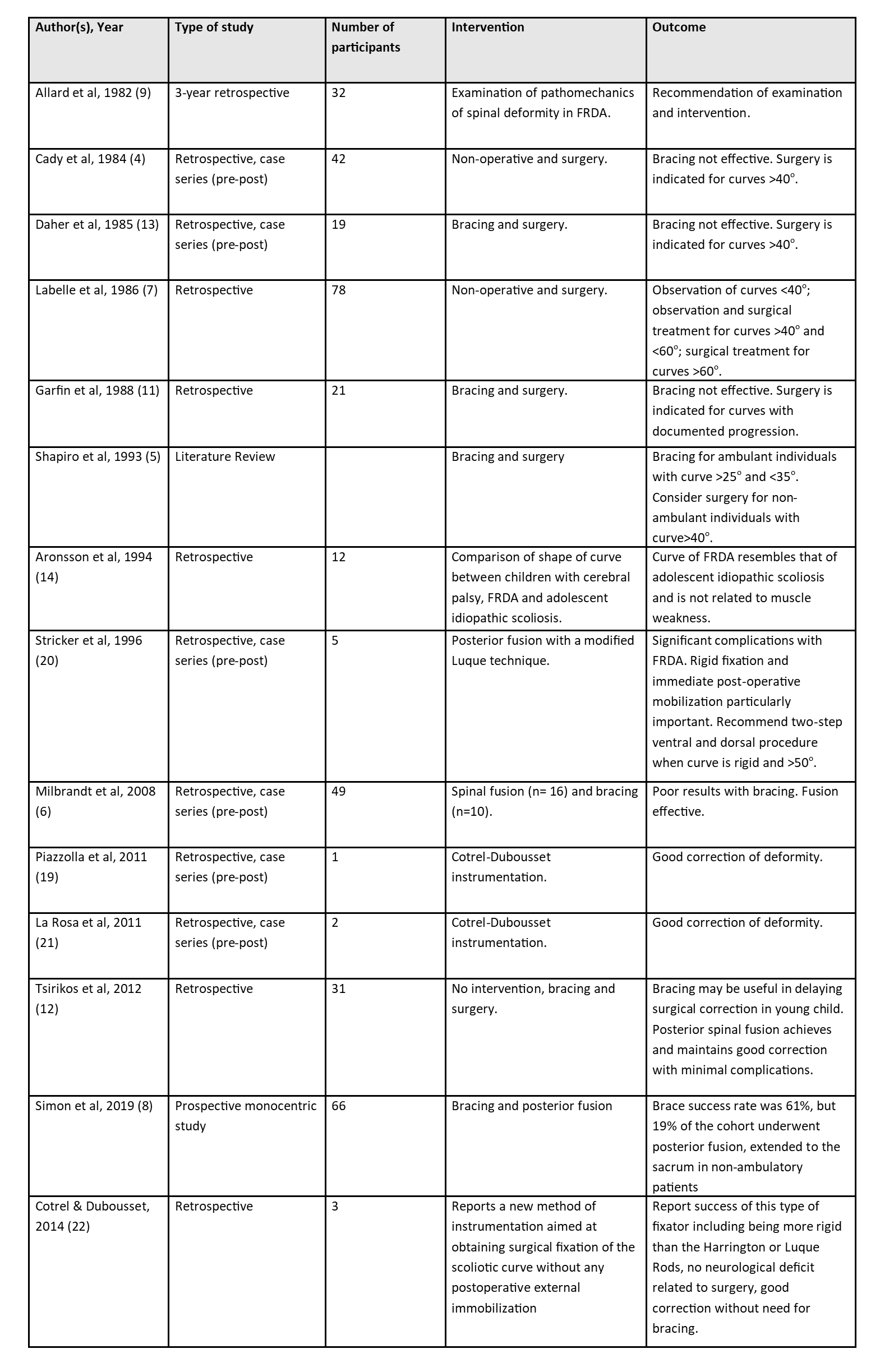
A literature search from 1957 to 2021 revealed 14 articles related to management of scoliosis in Friedreich ataxia. The majority of these studies are retrospective, with sample sizes ranging from 1 to 78 (see Table 9.1 for details of each study).
Table 9.1: Summary of studies related to management of scoliosis in Friedreich ataxia
The goal of intervention in individuals with FRDA is to prevent progression of scoliosis, improve posture and the capacity for upright stability in those who are ambulatory, improve balance, and reduce the reliance on external orthoses for postural control and pressure/pain relief in those who are non-ambulatory (8). In addition, prevention of secondary respiratory complications is a significant factor to consider in the management of scoliosis in FRDA (19). In both ambulatory and non-ambulatory groups, pain is a significant indicator for intervention and thus successful intervention may have a significant impact on quality of life for people with FRDA.
Most authors recommend observation of children with a curve between 20o and 40o; however, they suggest that if the curve progresses beyond 40o, intervention is indicated (4, 7). Intervention can be non-invasive, such as the use of bracing in the ambulatory individual or the use of customized seating to limit progression of rotation and lateral deviation of the spine in non-ambulatory individuals. Although the efficacy of bracing in controlling deformity has been questioned (6), bracing may be particularly valuable in the very young and compliant person with FRDA to slow down progression and delay surgical correction (12). Unfortunately, bracing may interfere with ambulation and breathing and thus compliance may be an issue (4, 6, 9, 13).
Consideration of surgical intervention for scoliosis should take into account the negative effects of Implant failure, risk of infection and risk of loss of mobility in the recovery phase post-operatively (8). The fusion level (e.g., extending fusion to the pelvis), in particular the mobility status and projected loss of ambulation of each individual, should also be considered. Finally, the risk of intraoperative complications such as fluid loss/overload and associated cardiac issues need to be considered (8). Simon and colleagues (8) reviewed the rate of scoliosis progression in a small cohort of 28 individuals with FRDA who were managed conservatively and noted conservative treatment such as bracing did not influence the per-year rate of progression. Whilst there is little literature reporting post-operative mobility, Simon and colleagues (8) did report those who were still ambulatory when undergoing surgical intervention (n=5) were still able to walk two to five years postoperatively. As indicated by Rummey and colleagues (3), loss of ambulation often coincides with the requirement for scoliosis surgery, which confounds interpretation of surgical outcomes in regards to ambulation status.
Posterior fusion may be considered for progressive curves greater than 40o in the child who is still growing (4, 7, 9). Milbrandt and colleagues (6) recommend consideration of surgery when the curves approach 50o. Stricker and colleagues (20) expanded the criteria to include those individuals who experience significant loss of balance while sitting, poor control of the head and difficulty complying with orthotic devices. Piazzolla and colleagues (19) proposed that indications for surgery should include deformity causing functional problems (poor sitting balance, difficulties with hygiene), or impingement of the rib cage on the pelvis or a deformity that could progress to create any of all of these problems. It has been recommended that the fusion area extend from T2 to L3 or L4 and the instrumentation contoured to accommodate the usual thoracic kyphosis and lumbar lordosis (5, 6). However, some individuals may benefit from a shorter fusion and those who are non-ambulatory may require a fusion to the pelvis. The decision to fuse and the nature of the fusion should be based on each individual case taking into consideration the severity of the deformity, mobility and associated risks (12).
Spinal deformities are corrected using a posterior instrumented spinal fusion with pedicle screw fixation. In some cases, pelvic fixation may be required. Standard, modern intraoperative neuromonitoring may not be possible in all children with FRDA who need spine deformity correction, so the surgical team must be prepared to perform a wake-up test.
Cardiopulmonary assessment is essential prior to consideration of surgery to ensure cardiac function is not compromised during the procedure and in the post-operative phase (23).
See Chapter 4 for assessment and management of cardiac issues.
It is important to delay surgery for as long as possible by use of conservative management. When the scoliosis has progressed in terms of curve magnitude, surgery should be considered after careful multidisciplinary evaluation (including cardiac function). In consideration of surgical management of scoliosis for individuals with FRDA, it is essential to consider issues related to complications and post-operative management. In addition, it is important to consider if, depending on the ambulation status of the patient, the fusion should be extended to the pelvis. Some studies reported post-operatively immobilization in orthoses for periods from 3 to 15 months (4, 13). Moreover, significant intraoperative blood loss may compound pre-existing cardiopulmonary issues (23); hence it is critical surgery is conducted in a facility with an intensive care unit (ICU) for initial post-operative care. Complications related to loss of mobility, de-conditioning, infection, failure of the implants, cardiopulmonary issues or death are reported in most studies. Post-operative requirements and availability in terms of acute community-based care and impact on life roles of the individual with FRDA (e.g., time off school, increase in level of dependency, possible deconditioning associated with post-operative recovery) need to be considered on a case-by-case basis. While there is some evidence that physical therapy may slow the progression and/or improve Cobb angles in idiopathic scoliosis (24), there is no evidence that such intervention would be effective in individuals with FRDA.
9.2.3 Conclusion
The available literature largely supports the role of surgery in correcting scoliosis in individuals with FRDA who demonstrate a curve >40o and in whom presence of a curve has a significant impact on health, independence, and quality of life. However, expert authors consider it is important to delay surgery for as long as possible by the use of conservative management. Bracing, while not proven to affect the prognosis of the deformity or the need for surgical correction, may be valuable in delaying surgical correction in the very young child. When the scoliosis has progressed in terms of Cobb angle and associated discomfort, surgery should be considered only after extensive pre-operative multidisciplinary evaluation, with particular attention to cardiorespiratory function. If surgery is considered, the need to extend fusion to the pelvis (depending on ambulation status of patient) should be assessed.
Surgery for scoliosis
QUESTION: Should surgery versus conservative therapy be used for scoliosis with Friedreich ataxia?
STRENGTH OF RECOMMENDATION: ↓LEVEL OF EVIDENCE: ⨁◯◯◯
RECOMMENDATION: We suggest surgery should not be used over conservative therapy for individuals with scoliosis and Friedreich ataxia. Expert opinion suggests that conservative therapy, including the use of bracing during the time of rapid growth in children/adolescents (age 10 to 16 years), may assist in avoiding or delaying surgery.
JUSTIFICATION: The expert authors consider it is important to delay surgery for scoliosis in individuals with Friedreich ataxia for as long as possible by use of conservative management. When the scoliosis has progressed in terms of Cobb angle and associated discomfort, surgery should be considered only after careful multidisciplinary evaluation (including cardiac function). If surgery is considered, the necessity or not to extend fusion to the pelvis should be assessed, depending on the ambulation status of patient.
SUBGROUP CONSIDERATION: This recommendation is for individuals with Friedreich ataxia with scoliosis. Ambulatory individuals with scoliosis are at risk of losing ambulation through the process of surgical intervention; therefore, those who are still ambulant may require particular consideration.
Evidence to Recommendation Table PDFAge and scoliosis surgery
QUESTION: Should age be considered versus none be used for scoliosis surgery with Friedreich ataxia?
STRENGTH OF RECOMMENDATION: ↑↑LEVEL OF EVIDENCE: ⨁◯◯◯
RECOMMENDATION: We recommend that age should be considered when contemplating scoliosis surgery for individuals with Friedreich ataxia.
JUSTIFICATION: Expert opinion suggests that the use of bracing during the time of rapid growth in children with scoliosis (age 10 to 16 years) may assist in avoiding surgery. For young children (before age 10 years), we recommend aiming to prevent progression of scoliosis with bracing rather than surgery, in an effort to avoid early spine fusion.
SUBGROUP CONSIDERATION: This recommendation is for individuals with Friedreich ataxia with scoliosis. Younger individuals require specific attention when considering scoliosis surgery or other treatments.
Evidence to Recommendation Table PDFCardiac status and scoliosis surgery
QUESTION: Should cardiac status versus none be used for stratifying scoliosis surgery with Friedreich ataxia?
STRENGTH OF RECOMMENDATION: ↑↑LEVEL OF EVIDENCE: ⨁◯◯◯
RECOMMENDATION: We recommend stratifying individuals with Friedreich ataxia according to cardiac status when considering scoliosis surgery.
JUSTIFICATION: Individuals with Friedreich ataxia and concurrent cardiac disease may be at greater risk of intra and post-operative complications related to fluid loss/overload and congestive cardiac failure. Individuals with Friedreich ataxia undergoing scoliosis surgery should undergo EKG, echocardiography and a cardiology consultation within a reasonable time frame prior to the surgery (e.g., 2 to 4 months prior) to evaluate left ventricular (LV) structure and left ventricular ejection fraction (LVEF). The surgical plan should incorporate a cardiac management plan in conjunction with the cardiologist.
SUBGROUP CONSIDERATION: This recommendation is for Individuals with Friedreich ataxia who require scoliosis surgery.
Evidence to Recommendation Table PDFIndividuals with Friedreich ataxia with a spinal curve between 20o and 40o and/or between the ages of 10 and 16 years should be observed for curve progression.
Bracing may not reduce or stop the progression of curves; however, it may be valuable in delaying surgical correction in the young child.
People with Friedreich ataxia with a scoliosis >40o may be considered appropriate for surgical correction.
Consideration should be given to delaying surgical intervention in ambulant individuals with Friedreich ataxia.
All people with Friedreich ataxia considered for scoliosis surgery require extensive pre-operative evaluation and planning regarding cardiac and pulmonary function.
Lay summary of clinical recommendations for scoliosis in Friedreich ataxia
Why these recommendations?
Scoliosis (curvature of the spine) occurs in most individuals with Friedreich ataxia. Scoliosis can be severe, where it happens at a young age (earlier than 10 years of age) and gets progressively worse over time, or it can be less severe and not get much worse over time.
These recommendations suggest that individuals with Friedreich ataxia should have a regular examination of the spine, particularly young people aged between 10 and 16 years. If a spinal curve is apparent, it should be observed over time to see if it gets worse.
The options for correcting a scoliosis are either to wear an external brace or undergo surgery. For young children (before age 10 years), we recommend aiming to prevent progression of scoliosis with bracing in the first instance, in an effort to avoid early spine fusion with surgery. While bracing may not reduce or stop the progression of the curve, it may be valuable in delaying surgery, particularly for young children or someone who is still able to walk.
If surgery for scoliosis is being considered, individuals with Friedreich ataxia and cardiac disease may be at greater risk of complications related to fluid loss/overload and congestive cardiac failure during or after surgery. Individuals with Friedreich ataxia undergoing scoliosis surgery should therefore have an EKG, echocardiography and a cardiology consultation within a reasonable time before the surgery.
What does this mean for you as a person living with Friedreich ataxia or caring for someone living with Friedreich ataxia?
It might be important for you to speak with your healthcare professional about Friedreich ataxia and management of spinal curves and what it means for you.
Who are these recommendations specifically for?
These recommendations are specifically for individuals with Friedreich ataxia and scoliosis.
Louise Corben, PhD
Principal Research Fellow, Murdoch Children’s Research Institute, Melbourne, Victoria, Australia
Email: louise.corben@mcri.edu.au
John M. (Jack) Flynn, MD
Richard M. Armstrong, Jr., Endowed Chair, Chief of Orthopaedic Surgery, The Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, USA
David Lynch, MD, PhD
Professor of Neurology and Pediatrics, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania, USA
Email: lynchd@mail.med.upenn.edu
2. Reetz K, Dogan I, Hohenfeld C, Didszun C, Giunti P, Mariotti C, et al. Nonataxia symptoms in Friedreich Ataxia: Report from the Registry of the European Friedreich’s Ataxia Consortium for Translational Studies (EFACTS). Neurology. 2018;91(10):e917-e30.
3. Rummey C, Flynn JM, Corben LA, Delatycki MB, Wilmot G, Subramony SH, et al. Scoliosis in Friedreich’s ataxia: longitudinal characterization in a large heterogeneous cohort. Ann Clin Transl Neurol. 2021;8(6):1239-50.
4. Cady RB, Bobechko WP. Incidence, natural history, and treatment of scoliosis in Friedreich’s ataxia. J Pediatr Orthop. 1984;4(6):673-6.
5. Shapiro F, Specht L. The diagnosis and orthopaedic treatment of childhood spinal muscular atrophy, peripheral neuropathy, Friedreich ataxia, and arthrogryposis. J Bone Joint Surg Am. 1993;75(11):1699-714.
6. Milbrandt TA, Kunes JR, Karol LA. Friedreich ataxia and scoliosis. The experience of two institutions. Journal of Pediatric Orthopaedics. 2008;28(2):234-8.
7. Labelle H, Tohme S, Duhaime M, Allard P. Natural history of scoliosis in Friedreich’s ataxia. Journal of Bone & Joint Surgery – American Volume. 1986;68(4):564-72.
8. Simon AL, Meyblum J, Roche B, Vidal C, Mazda K, Husson I, et al. Scoliosis in Patients With Friedreich Ataxia: Results of a Consecutive Prospective Series. Spine Deform. 2019;7(5):812-21.
9. Allard P, Dansereau J, Thiry PS, Geoffroy G, Raso JV, Duhaime M. Scoliosis in Friedreich’s ataxia. Can J Neurol Sci. 1982;9(2):105-11.
10. Delatycki MB, Paris DB, Gardner RJ, Nicholson GA, Nassif N, Storey E, et al. Clinical and genetic study of Friedreich ataxia in an Australian population. Am J Med Genet. 1999;87(2):168-74.
11. Garfin SR, Leach J, Mubarak SJ, Schultz P. Experimental approach–and literature review–of spinal care in adults with a neuromuscular disorder. J Spinal Disord. 1988;1(3):202-5.
12. Tsirikos AI, Smith G. Scoliosis in Friedreich’s ataxia. The Journal of Bone and Joint Surgery. 2012;94(B):684-9.
13. Daher YH, Lonstein JE, Winter RB, Bradford DS. Spinal deformities in patients with Friedreich ataxia: a review of 19 patients. J Pediatr Orthop. 1985;5(5):553-7.
14. Aronsson DD, Stokes IA, Ronchetti PJ, Labelle HB. Comparison of curve shape between children with cerebral palsy, Friedreich’s ataxia, and adolescent idiopathic scoliosis. Dev Med Child Neurol. 1994;36(5):412-8.
15. Delatycki MB, Holian A, Corben L, Rawicki HB, Blackburn C, Hoare B, et al. Surgery for equinovarus deformity in Friedreich’s ataxia improves mobility and independence. Clin Orthop Relat Res. 2005;430:138-41.
16. Keenan MA. The management of spastic equinovarus deformity following stroke and head injury. Foot Ankle Clin. 2011;16(3):499-514.
17. Maring JR, Croarkin E. Presentation and progression of Friedreich ataxia and implications for physical therapist examination. Phys Ther. 2007;87(12):1687-96.
18. Cobb JR. Outline for the study of scoliosis. Instr Course Lect. 1948;5:261-75.
19. Piazzolla A, Solarino G, De Giorgi S, Mori CM, Moretti L, De Giorgi G. Cotrel-Dubousset instrumentation in neuromuscular scoliosis. Eur Spine J. 2011;20 Suppl 1:S75-84.
20. Stricker U, Moser H, Aebi M. Predominantly posterior instrumentation and fusion in neuromuscular and neurogenic scoliosis in children and adolescents. Eur Spine J. 1996;5(2):101-6.
21. La Rosa G, Giglio G, Oggiano L. Surgical treatment of neurological scoliosis using hybrid construct (lumbar transpedicular screws plus thoracic sublaminar acrylic loops). Eur Spine J. 2011;20 Suppl 1:S90-4.
22. Cotrel Y, Dubousset J. A new technic for segmental spinal osteosynthesis using the posterior approach. Orthop Traumatol Surg Res. 2014;100(1):37-41.
23. Payne RM, Wagner GR. Cardiomyopathy in Friedreich ataxia: clinical findings and research. J Child Neurol. 2012;27(9):1179-86.
24. Fusco C, Zaina F, Atanasio S, Romano M, Negrini A, Negrini S. Physical exercises in the treatment of adolescent idiopathic scoliosis: an updated systematic review. Physiother Theory Pract. 2011;27(1):80-114.
25. Suat E, Fatma U, Nilgun B. The effects of dynamic ankle-foot orthoses on functional ambulation activities, weight bearing and spatio-temporal characteristics of hemiparetic gait. Disabil Rehabil. 2011;33(25-26):2605-11.
26. Näslund A, Jesinkey K, Hirschfeld H, von Wendt L, Sundelin G. Effects of dynamic ankle-foot orthoses on standing in children with severe spastic diplegia. International Journal of Therapy and Rehabilitation. 2005;12:200-7.
27. Chen CC, Hong WH, Wang CM, Chen CK, Wu KP, Kang CF, et al. Kinematic features of rear-foot motion using anterior and posterior ankle-foot orthoses in stroke patients with hemiplegic gait. Arch Phys Med Rehabil. 2010;91(12):1862-8.
28. Cruz TH, Dhaher YY. Impact of ankle-foot-orthosis on frontal plane behaviors post-stroke. Gait Posture. 2009;30(3):312-6.
29. Fatone S, Gard SA, Malas BS. Effect of ankle-foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch Phys Med Rehabil. 2009;90(5):810-8.
30. Kobayashi T, Leung AK, Akazawa Y, Hutchines SW. Design and effect of ankle-foot orthoses proposed to influence muscle tone: a review. J Prosthet Orthot. 2011;23:52-7.
These Guidelines are systematically developed evidence statements incorporating data from a comprehensive literature review of the most recent studies available (up to the Guidelines submission date) and reviewed according to the Grading of Recommendations, Assessment Development and Evaluations (GRADE) framework © The Grade Working Group.
This chapter of the Clinical Management Guidelines for Friedreich Ataxia and the recommendations and best practice statements contained herein were endorsed by the authors and the Friedreich Ataxia Guidelines Panel in 2022.
It is our expectation that going forward individual topics can be updated in real-time in response to new evidence versus a re-evaluation and update of all topics simultaneously.

