Topic 16.2. The role of digital and assistive technologies in improving independence
This chapter of the Clinical Management Guidelines for Friedreich Ataxia and the recommendations and best practice statements contained herein were endorsed by the authors and the Friedreich Ataxia Guidelines Panel in 2022.
Topic Contents
16.2 The role of digital and assistive technologies in improving independence
16.2.1 Health monitoring and self-management
16.2.2 Communication aids
16.2.3 Environmental control
16.2.4 Mobility aids
16.2.5 Compensatory techniques
16.2.6 Restorative techniques
Disclaimer / Intended Use / Funding
Disclaimer
The Clinical Management Guidelines for Friedreich ataxia (‘Guidelines’) are protected by copyright owned by the authors who contributed to their development or said authors’ assignees.
These Guidelines are systematically developed evidence statements incorporating data from a comprehensive literature review of the most recent studies available (up to the Guidelines submission date) and reviewed according to the Grading of Recommendations, Assessment Development and Evaluations (GRADE) framework © The Grade Working Group.
Guidelines users must seek out the most recent information that might supersede the diagnostic and treatment recommendations contained within these Guidelines and consider local variations in clinical settings, funding and resources that may impact on the implementation of the recommendations set out in these Guidelines.
The authors of these Guidelines disclaim all liability for the accuracy or completeness of the Guidelines, and disclaim all warranties, express or implied to their incorrect use.
Intended Use
These Guidelines are made available as general information only and do not constitute medical advice. These Guidelines are intended to assist qualified healthcare professionals make informed treatment decisions about the care of individuals with Friedreich ataxia. They are not intended as a sole source of guidance in managing issues related to Friedreich ataxia. Rather, they are designed to assist clinicians by providing an evidence-based framework for decision-making.
These Guidelines are not intended to replace clinical judgment and other approaches to diagnosing and managing problems associated with Friedreich ataxia which may be appropriate in specific circumstances. Ultimately, healthcare professionals must make their own treatment decisions on a case-by-case basis, after consultation with their patients, using their clinical judgment, knowledge and expertise.
Guidelines users must not edit or modify the Guidelines in any way – including removing any branding, acknowledgement, authorship or copyright notice.
Funding
The authors of this document gratefully acknowledge the support of the Friedreich Ataxia Research Alliance (FARA). The views and opinions expressed in the Guidelines are solely those of the authors and do not necessarily reflect the official policy or position of FARA.
16.2 The role of digital and assistive technologies in improving independence
Ellen W. Goh, Manuela Corti, Kathrin Reetz, Sub H. Subramony and Louise Corben
Interventions aimed at maintaining or improving independence in people with FRDA can either be compensatory, that is interventions that improve function by compensating for the underlying deficit; or restorative, that is interventions that aim to facilitate restoration of function by adaptation and recovery within the neuro‐musculoskeletal system (1).
As a consequence of disease progression individuals with FRDA become increasingly dependent on adaptive equipment. Symptoms including ataxia, muscle weakness, spasticity and bony changes such as scoliosis and foot deformity interfere with the ability to mobilize, attend to personal daily tasks and to stand and transfer independently, the latter of which is a significant contributor to ongoing maintenance of independence. Given there is limited evidence regarding the provision of adaptive equipment for people with FRDA, clinical reasoning underlying provision of adaptive equipment is largely based on evidence from similar progressive, neurological conditions. It is critical however that the clinician prescribing the equipment is familiar with the particular issues related to FRDA and experienced in the adaptive equipment prescribed. In particular, the prescription of the first wheelchair can be seen as a significant milestone in the progression of the condition; hence, ensuring active involvement of both the client and parents (if appropriate) is critical (2). Here, mobility should not be the only focus of attention, but also possible neuromuscular deformities such as poor posture due to the presence of scoliosis (e.g., adjustment of a seating system, with for example, foam or gel inserts, to improve seated posture).
16.2.1 Health monitoring and self-management
Health monitoring and alert devices have becoming increasingly available in recent years; however, their adoption into real-life use has been low in like conditions (3). Examples include phone applications that track physical activity, prompt/remind for medication, monitor clinical indicators (e.g., heart rate) or provide tools for self-management strategies (sleep, fatigue management). Digital tracking and monitoring tools are used to support self-management and personalized health care in like conditions; however, the acceptance of these apps and devices depends on the person experiencing the value of the device and being well equipped to use them (3). Further development of these tools is required to ensure they are adaptable to a person’s own situation, there is support to understand the information gathered and there are links into clinical treatment plans (3). For people with FRDA there are a number of medical co-morbidities which might be better monitored or managed through the use of digital assistive technology. Smart watches that can monitor heart rate, sleep cycles or prompts for medication regimes may be useful. Technology such as blood glucose monitoring systems may also be helpful in a person managing their FRDA-related diabetes (see Chapter 10, section 10.1). Applications to record, track and prompt healthy lifestyle behaviors or therapy tools for physical exercise can be useful to provide a person with FRDA an opportunity to engage in self-management. Given there is limited evidence for the use of these systems, it is vital that any digital or assistive technology be explored with appropriate clinical reasoning and full involvement of the person with FRDA to ensure they are well equipped to use the device or technology.
16.2.2 Communication aids
There is limited research in like conditions related to assistive technology for use in communication and to facilitate workplace participation. One study in amyotrophic lateral sclerosis, a like condition with progressively deteriorating expressive communication and upper limb function, suggests that early use of tablet-based assistive technology for communication is beneficial and has positive impacts on quality of life, particularly as the condition progresses and more complex alternative strategies are required (4). For people with FRDA, customized communication devices that compensate for upper limb, vision, hearing and/or speech deficits may enhance communication and workplace opportunities (see Chapter 3.5).
16.2.3 Environmental control
Environmental control is becoming more mainstream with the development and widespread commercial availability of technical systems such as Apple Siri, Google Home and Amazon Alexa. These integrated devices allow users to control aspects of their home environment such as lighting, heating, answering the door and controlling appliances via their phone or tablet, making it easier for disabled persons to live independently. Access to this technology is becoming easier thanks to particular brands of phone or tablet that already have inbuilt Apps for such function at a reasonable cost. Use of such freely available environmental control devices in addition to more customized and specially designed systems for people with FRDA may enable greater independence within a person’s home.
16.2.4 Mobility aids
Customized assistive technology for mobility includes modified vehicles, wheelchairs, traction devices, transfer devices (sling or standing hoists, sit to stand aids such as Sara Stedy [https://www.arjo.com/int/products/patient-handling/standing-and-raising-aid/sara-stedy/], ETAC turners [https://www2.etac.com/en-us/products/product-archive/manual-transfer/etac-turner/]), walkers, adaptive seating and positioning aids. These devices can assist a person to mobilize, transfer, access the home or community and participate in all aspects of daily life.
Due to progressive muscle weakness, ataxia, spasticity and other neuromuscular changes the needs for assistive technology will probably change over time. There may be a progression from transfers in standing/stepping to the use of standing/sling or track hoists and lifters to enable safe transfers in a person’s environment. A thorough assessment of a person’s functional abilities within the context of their own environment is crucial to selecting the most appropriate device for mobility, transfers and seating. A focus on maintaining active participation in mobility and transfers is critical to maintaining engagement of muscles, which is important in maintaining muscle strength. A sling hoist removes any active participation of the person’s upper body, core or lower body and is frequently used from a lying or supported sitting position. Alternatively, a standing hoist is used from a sitting position with the sling just around the middle of the body and this allows engagement of upper limb and lower limbs in the process of helping with standing. Preserving active use of upper limbs, core and lower limbs in any way is important for a person with FRDA and the use of transfers is a further opportunity for these muscles to be engaged on a daily basis. Despite the sometimes unconventional techniques for transfers, a balance between risk and independence must be considered. Moving too quickly from a standing transfer to a hoist can have unintended consequences in addition to further loss of lower limb strength, for core strength, foot and ankle muscle length and upper limb function.
Individuals with FRDA benefit from the provision of grab rails to assist in attending to activities of daily living. Given that ataxia is a core impairment, it is essential that grab rails be correctly positioned to ensure that during the transfer the person is able to maintain their center of gravity over their knees and feet. As such, grab rails positioned to facilitate pulling up, rather than pushing up may be of more benefit. Likewise, provision of wheeled commode/shower chairs requires customization to the specific requirements of a person with FRDA including stability and ease of maneuverability and transfer. This may include lowering the seat height to facilitate safe transfers, utilizing smaller seat apertures and ensuring an appropriate seat width to avoid extraneous trunk movement while in use.
16.2.5 Compensatory techniques
Compensatory techniques include interventions such as the use of weighted and adaptive equipment such as specialized cutlery, feeding and writing implements that feature both weighted, non‐slip and larger grips (5, 6) and weighting of the distal component of the limb during activity (7-10). The use of simple strategies to decompose multi‐joint movements to more accurate single joint movements (1, 11), minimize reaching movements and stabilize proximal joints (12) have also been proposed. Practically, this includes stabilizing the elbows on the table while feeding oneself, sliding the hand on the table to facilitate grasp instead of grasping in space, use of orthotics to stabilize joints (in particular the wrist), using two hands to grasp objects or using one hand to stabilize the other while manipulating an object. Training in independence tasks may also consider the significance of visuomotor or proprioceptive loss on functional capacity. People with FRDA may use vision to compensate for sensory impairment; however, the inherent delay in using visual feedback to correct motor performance needs to be factored into training and provision of equipment (e.g., programming of motorized wheelchairs).
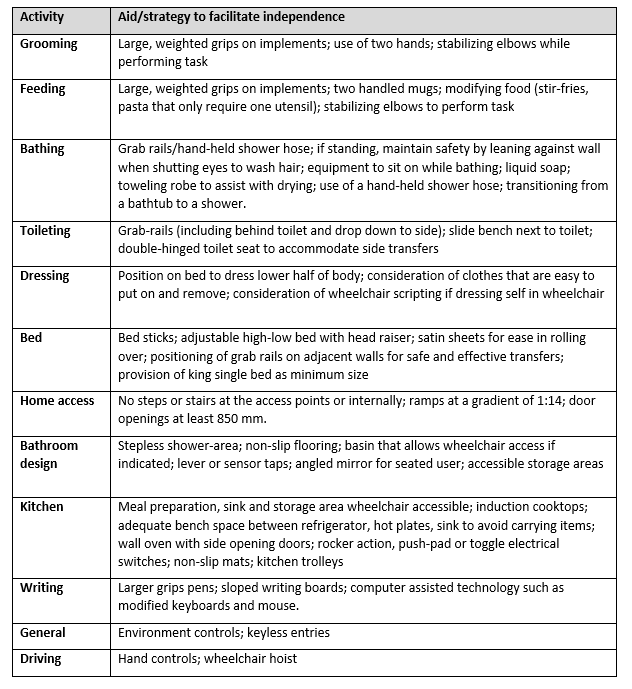
As mentioned, a detailed assessment of functional capacity in the context of the individual’s everyday environment such as home, work or community is critical to developing appropriate strategies to improve independence. The goals of intervention aimed at maximizing function in each environmental context can be incorporated into subsequent strategies and modifications to facilitate independence. Clinical reasoning is essential to avoid a prescriptive approach to the provision of adaptive equipment. For example, it is of greater benefit if people with ataxia are able to pull up, rather than push up on grab rails in order to maintain the center of gravity over their feet and thus ensure safety while transferring. Such clinical reasoning is necessary in most situations when providing adaptive equipment and modification of environment. Table 16.1 provides a summary of compensatory techniques for specific activities of daily living.
Table 16.1: Suggested interventions/aids to facilitate independence in daily activities
16.2.6 Restorative techniques
Restorative techniques include the use of physical rehabilitation, relaxation and biofeedback (13-15). However, these are not widely used in clinical practice for people with FRDA.
Assistive technology for mobility
QUESTION: Should customized assistive technology for mobility (e.g., modified vehicles, wheelchair, transfer devices, walkers, adaptive seating and positioning) versus non-use be used for individuals with impaired independent gait/mobility with Friedreich ataxia?
[sg_popup id=”587″ event=”click”] [/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[sg_popup id=”658″ event=”click”] [/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
[/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
RECOMMENDATION: For individuals with Friedreich ataxia with impaired independent gait/mobility, we suggest the use of customized assistive technology for mobility (e.g., modified vehicle, wheelchair, transfer devices, walkers, and adaptive seating and positioning) to enhance independence in mobility, quality of life, and social and occupational participation, and to reduce falls.
JUSTIFICATION: Despite the low level of evidence in like conditions, expert clinicians who provide clinical care for individuals with Friedreich ataxia agree that the use of customized assistive technology for mobility can benefit independence in mobility, quality of life, and social and occupational participation, and reduce falls.
SUBGROUP CONSIDERATION: This recommendation is specifically for individuals with Friedreich ataxia with impaired independent gait/mobility. The guideline expert panel considers that all individuals with Friedreich ataxia might benefit from the use of digital and assistive technology.
Evidence to Recommendation Table PDFPersonal care and environmental control
QUESTION: Should customized assistive technology (personal care technology, environmental control [iPAD, home APPs, smart watches], ALEXA/ SIRI) versus non-use be used for individuals with impaired upper limb functionality with Friedreich ataxia?
[sg_popup id=”587″ event=”click”] [/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[sg_popup id=”658″ event=”click”] [/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
[/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
RECOMMENDATION: For individuals with Friedreich ataxia with impaired upper limb functionality, we suggest the use of customized assistive technology for personal care and environmental control (e.g., iPad, home apps, smart watches, Alexa/Siri) to enhance independence in daily activities, quality of life, and social and occupational participation.
JUSTIFICATION: Despite the low level of evidence in only one like condition, expert clinicians who provide clinical care for individuals with Friedreich ataxia agree that customized assistive technology for personal care can benefit independence in daily activities, quality of life, and social and occupational participation in individuals with Friedreich ataxia.
SUBGROUP CONSIDERATION: This recommendation is specifically for individuals with Friedreich ataxia with impaired upper limb functionality. The guideline expert panel considers that all individuals with Friedreich ataxia might benefit from the use of digital and assistive technology.
Evidence to Recommendation Table PDFHealth monitoring
QUESTION: Should health monitoring/alert devices (e.g., monitoring heart rate, steps, sleep, ECG, activity, healthy eating, medication, glucose for diabetes) versus non-use be used for individuals with fatigue, fall risk, poor sleep, diabetes, etc, with Friedreich ataxia?
[sg_popup id=”587″ event=”click”] [/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[sg_popup id=”658″ event=”click”] [/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
[/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
RECOMMENDATION: For individuals with Friedreich ataxia and fatigue, a risk of falls, poor sleep, diabetes and/or cardiomyopathy, we suggest the use of health monitoring/alert devices (e.g., monitoring heart rate, steps, sleep, ECG, activity, healthy eating, medication, glucose for Friedreich ataxia-related diabetes) to enhance independence in daily activities and quality of life and improve medication control.
JUSTIFICATION: Despite the low level of evidence, expert clinicians who provide clinical care for individuals with Friedreich ataxia agree that customized assistive technology for health monitoring can benefit independence in daily activities, quality of life, number of hospitalizations, sleep, diabetes and medication control in individuals with Friedreich ataxia.
SUBGROUP CONSIDERATION: This recommendation is particularly relevant to individuals with Friedreich ataxia who report fatigue or poor sleep, are at risk of falls, and/or have diabetes or cardiomyopathy.
Evidence to Recommendation Table PDFCommunication and workplace assistance
QUESTION: Should customized assistive technology for communication and to expand workplace opportunities (e.g., writing, speech, computer use, tablets, workplace design [adaptive seating and positioning], vision and hearing) versus non-use be used for individuals with impaired communicating ability and workplace difficulties with Friedreich ataxia?
[sg_popup id=”587″ event=”click”] [/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[/sg_popup]STRENGTH OF RECOMMENDATION: ↑
[sg_popup id=”658″ event=”click”] [/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
[/sg_popup]LEVEL OF EVIDENCE: ⨁◯◯◯
RECOMMENDATION: For individuals with Friedreich ataxia with impaired communication and workplace difficulties, we suggest the use of customized assistive technology for communication and the workplace (e.g., writing, speech, computer use, tablets, workplace design [adaptive seating and positioning], vision and hearing) to enhance independence in communication, improve quality of life and increase occupational participation.
JUSTIFICATION: Despite the low level of evidence in like conditions, expert clinicians who provide clinical care for individuals with Friedreich ataxia agree that customized assistive technology for communication can benefit independence in communication, quality of life and occupational participation in individuals with Friedreich ataxia, particularly in the later stage of the disease.
SUBGROUP CONSIDERATION: The provision of customized assistive technology is particularly relevant to individuals with advanced Friedreich ataxia who may have concurrent issues related to upper limb ataxia, visual difficulties and eye movement problems.
Evidence to Recommendation Table PDFCompensatory or remedial interventions with digital and assistive technology may improve independence for individuals with Friedreich ataxia.
Prescription of a manual or powered wheelchair or scooter should be preceded by an assessment of the home/school/work and community environment the equipment will be used in.
A comprehensive prescription of a manual or powered wheelchair or scooter should be completed by a qualified clinician familiar with the specific issues related to Friedreich ataxia.
A validated assessment and evaluation tool for wheelchair and seating prescription may be used to guide the process of prescription and evaluation.
In prescribing a manual wheelchair and seating system, functional capacity should not be impeded for the sake of an anatomically correct seated posture.
Appropriate training should be provided for the safe use of a wheelchair or scooter in the home or community environment.
Suitability of the seating and wheelchair system should be evaluated on an annual basis in adults and biannually in children.
Lay summary of clinical recommendation for digital and assistive technologies in Friedreich ataxia
Why these recommendations?
These recommendations are about the use of digital and assistive technologies such as modified wheelchairs, adaptive seating, environmental controls, apps and smart watches. These technologies may help individuals with Friedreich ataxia with work, leisure, social and daily activities that involve communication, mobility and upper limb function. They may also be useful for individuals for whom it is important to maintain health and well-being, such as for management of diabetes or maintaining healthy eating.
Due to a lack of studies, there is little direct evidence showing the benefits of using digital and assistive technologies in individuals with Friedreich ataxia. However, the clinical experience of the authors and published research in other neurological conditions supports the consideration of using such technologies.
What does this mean for you as a person living with Friedreich ataxia or caring for someone living with Friedreich ataxia?
It might be important for you to talk to your allied health and medical clinicians to see if the use of digital and assistive technologies may be appropriate for you.
Who are these recommendations specifically for?
These recommendations are relevant to all individuals with Friedreich ataxia, particularly those who have lived with the condition for a long time and have many inter-related issues that may interfere with independence, such as speech, mobility and upper limb problems.
Louise Corben, PhD
Principal Research Fellow, Murdoch Children’s Research Institute, Melbourne, Victoria, Australia
Email: louise.corben@mcri.edu.au
Manuela Corti, P.T., PhD
Assistant Professor, University of Florida, Gainesville, Florida, USA
Email: m.corti@peds.ufl.edu
Ellen W. Goh, BAppSc(OccTherapy)
Neurosciences Clinical Lead Occupational Therapist, Monash Health, Melbourne, Victoria, Australia
Email: ellen.goh@monashhealth.org
Kathrin Reetz, MD
Professor for Translational Neurodegeneration, Department of Neurology, RWTH Aachen University, Aachen, NRW, Germany
Email: kreetz@ukaachen.de
Sub H. Subramony, MD
Professor of Neurology and Pediatrics, University of Florida College of Medicine, Gainesville, Florida, USA
Email: s.subramony@neurology.ufl.edu
1. Marsden J, Harris C. Cerebellar ataxia: pathophysiology and rehabilitation. Clin Rehabil. 2011;25(3):195-216.
2. Clark J, Shona M, Morrow M. Wheelchair postural support for young people with progressive neuromuscular disorders. International Journal of Therapy and Rehabiliation 2004;11(8):365-73.
3. Wendrich K, van Oirschot P, Martens MB, Heerings M, Jongen PJ, Krabbenborg L. Toward digital self-monitoring of multiple sclerosis: investigating first experiences, needs, and wishes of people with MS. Int J MS Care. 2019;21(6):282-91.
4. Londral A, Pinto A, Pinto S, Azevedo L, De Carvalho M. Quality of life in amyotrophic lateral sclerosis patients and caregivers: Impact of assistive communication from early stages. Muscle Nerve. 2015;52(6):933-41.
5. Broadhurst MJ, Stammers CW. Mechanical feeding aids for patients with ataxia: design considerations. J Biomed Eng. 1990;12(3):209-14.
6. Wyckoff E. The spoon phase is another option for self-feeding. Am J Occup Ther. 1993;47(9):851.
7. Morgan MH. Ataxia and weights. Physiotherapy. 1975;61(11):332-4.
8. Morrice BL, Becker WJ, Hoffer JA, Lee RG. Manual tracking performance in patients with cerebellar incoordination: effects of mechanical loading. Can J Neurol Sci. 1990;17(3):275-85.
9. Dahlin-Webb SR. A weighted wrist cuff. Am J Occup Ther. 1986;40(5):363-4.
10. Sanes JN, LeWitt PA, Mauritz KH. Visual and mechanical control of postural and kinetic tremor in cerebellar system disorders. J Neurol Neurosurg Psychiatry. 1988;51(7):934-43.
11. Bastian AJ. Mechanisms of ataxia. Phys Ther. 1997;77(6):672-5.
12. Gillen G. Improving activities of daily living performance in an adult with ataxia. Am J Occup Ther. 2000;54(1):89-96.
13. Davis AE, Lee RG. EMG biofeedback in patients with motor disorders: an aid for co-ordinating activity in antagonistic muscle groups. Can J Neurol Sci. 1980;7(3):199-206.
14. Guercio J, Chittum R, McMorrow M. Self-management in the treatment of ataxia: a case study in reducing ataxic tremor through relaxation and biofeedback. Brain Inj. 1997;11(5):353-62.
15. Guercio JM, Ferguson KE, McMorrow MJ. Increasing functional communication through relaxation training and neuromuscular feedback. Brain Inj. 2001;15(12):1073-82.
16. Mortenson WB, Miller WC, Miller-Pogar J. Measuring wheelchair intervention outcomes: Development of the wheelchair outcome measure. Disabil rehabilitation: Assist Technol. 2007;2(5):275-85.
17. Richardson M, Frank AO. Electric powered wheelchairs for those with muscular dystrophy: problems of posture, pain and deformity. Disabil Rehabil Assist Technol. 2009;4(3):181-8.
18. Cooper RA, Koontz AM, Ding D, Kelleher A, Rice I, Cooper R. Manual wheeled mobility–current and future developments from the human engineering research laboratories. Disabil Rehabil. 2010;32(26):2210-21.
19. Burgman I. The trunk/spine complex and wheelchair seating for children: A literature review Aust Occup Ther J. 1994;41(3):123-32.
20. Stockton L, Gebhardt KS, Clark M. Seating and pressure ulcers: clinical practice guideline. J Tissue Viability. 2009;18(4):98-108.
21. McCarthy RE. Management of neuromuscular scoliosis. Orthop Clin North Am. 1999;30(3):435-49.
22. Holmes KJ, Michael SM, Thorpe SL, Solomonidis SE. Management of scoliosis with special seating for the non-ambulant spastic cerebral palsy population – a biomechanical study. Clinical Biomechanics. 2003;18:480-7.
23. Ferrarin M, Andreoni G, Pedotti A. Comparative biomechanical evaluation of different wheelchair seat cushions. J Rehabil Res Dev. 2000;37(3):315-24.
24. De Souza LH, Frank AO. Rare diseases: matching wheelchair users with rare metabolic, neuromuscular or neurological disorders to electric powered indoor/outdoor wheelchairs (EPIOCs). Disabil Rehabil. 2016;38(16):1547-56.
25. Parent F, Dansereau J, Lacoste M, Aissaouri R. Evaluation of the new flexible contour backrest for wheelchairs J Rehabil Res Dev. 2000;37(3):325-33.
26. Liu HY, Pearlman J, Cooper R, Hong EK, Wang H, Salatin B, et al. Evaluation of aluminum ultralight rigid wheelchairs versus other ultralight wheelchairs using ANSI/RESNA standards. J Rehabil Res Dev. 2010;47(5):441-55.
27. Freixes O, Fernandez SA, Gatti MA, Crespo MJ, Olmos LE, Rubel IF. Wheelchair axle position effect on start-up propulsion performance of persons with tetraplegia. J Rehabil Res Dev. 2010;47(7):661-8.
28. Salminen AL, Brandt A, Samuelsson K, Toytari O, Malmivaara A. Mobility devices to promote activity and participation: a systematic review. J Rehabil Med. 2009;41(9):697-706.
29. Mountain AD, Kirby RL, Smith C. Skills training: an important component of powered wheelchair use. Clin Rehabil. 2009;23(3):287.
30. Mateo I, Llorca J, Volpini V, Corral J, Berciano J, Combarros O. Expanded GAA repeats and clinical variation in Friedreich’s ataxia. Acta Neurol Scand. 2004;109(1):75-8.
31. La Pean A, Jeffries N, Grow C, Ravina B, Di Prospero NA. Predictors of progression in patients with Friedreich ataxia. Mov Disord. 2008;23(14):2026-32.
32. Delatycki MB, Paris DB, Gardner RJ, Nicholson GA, Nassif N, Storey E, et al. Clinical and genetic study of Friedreich ataxia in an Australian population. Am J Med Genet. 1999;87(2):168-74.
These Guidelines are systematically developed evidence statements incorporating data from a comprehensive literature review of the most recent studies available (up to the Guidelines submission date) and reviewed according to the Grading of Recommendations, Assessment Development and Evaluations (GRADE) framework © The Grade Working Group.
This chapter of the Clinical Management Guidelines for Friedreich Ataxia and the recommendations and best practice statements contained herein were endorsed by the authors and the Friedreich Ataxia Guidelines Panel in 2022.
It is our expectation that going forward individual topics can be updated in real-time in response to new evidence versus a re-evaluation and update of all topics simultaneously.